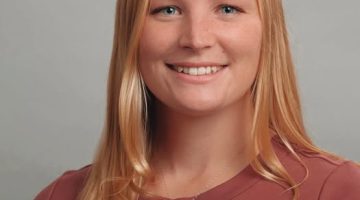
F31 Award Announcement!
The National Institutes of Health awarded GSBSE Ph.D. candidate Amanda Ignacz the prestigious Ruth L. Kirschstein Predoctoral Individual National Research Service Award for her work with neuromuscular disease. Amanda is the first graduate student working in Orono at UMaine to receive this award. This nationally competitive award honors and invests in pre-doctoral students by helping […]
Read more